Material below is adapted from the SfN Short Course Purification and Culture Methods for Astrocytes, by Shane Liddelow, PhD. Short Courses are day-long scientific trainings on emerging neuroscience topics and research techniques held the day before SfN’s annual meeting.
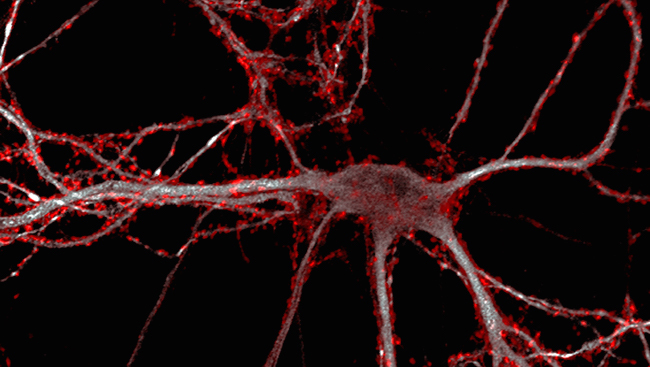
Astrocytes are star-shaped glial cells that can clear debris, form scars, and take a number of other actions in response to a variety of central nervous system (CNS) problems, such as brain tumors, stroke, and neurodegenerative disease. But alongside beneficial effects, reactive astrocytes may also have a negative impact on CNS health.
Access to the full article is available to SfN members.
Neuronline is a benefit of SfN membership. Renew your membership now to make sure you don’t lose access.