Drugs That Promote Remyelination Could Help Treat Multiple Sclerosis
Material below is adapted from the SfN Short Course Drug-Based Modulation of Endogenous Stem Cells Promotes Functional Remyelination In Vivo, by Fadi Najm, et al. Short Courses are daylong scientific trainings on emerging neuroscience topics and research techniques held the day before SfN’s annual meeting.
Working like the insulation coating electrical wires, myelin — the fatty substance sheathing the thin fiber projecting from the neuronal cell body — protects those axons and supports efficient nerve transmission.
Multiple sclerosis (MS) arises when the immune system attacks myelin causing communication problems between the brain and the rest of the body. MS is characterized by both damage to the myelin sheath (demyelination) and a failure to repair the damaged myelin (remyelination). Without the protective myelin coating, messages traveling along nerve fibers may be slowed or stopped, and, over time, the axons and cell bodies of neurons can also become damaged.
Current treatments for MS exclusively target the immune system to prevent or slow down further demyelination. Although immunomodulatory drugs can ease inflammation in patients with MS, none of them prevents the progression of this chronic disease, largely due to their inability to stop or reverse the failure of remyelination.
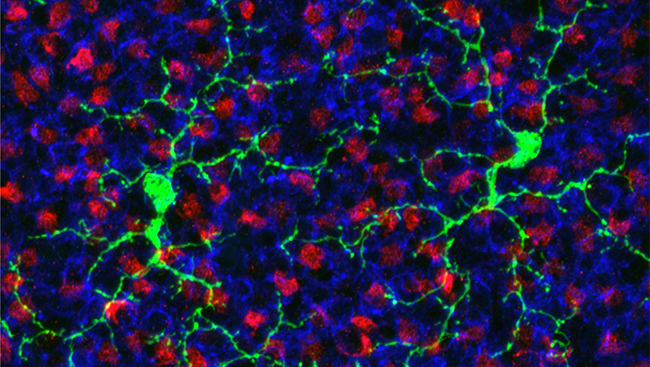
Recently, more research has focused on attempting to find treatments that work by promoting repair of damaged myelin. Remyelination is performed by nerve cells known as oligodendrocytes, which mature from oligodendrocyte progenitor cells (OPCs) in the central nervous system. While MS patients possess abundant OPCs, they fail to differentiate into oligodendrocytes and cannot help repair damaged myelin. Promoting OPC differentiation is a promising target for drug treatment.
To identify drugs that could be repurposed as remyelinating therapeutics, researchers screened a library of small molecules, assessing their ability to drive the differentiation of OPCs into oligodendrocytes. Two drugs approved by FDA, miconazole and clobetasol, demonstrated new functions: the ability to modulate OPC maturation, enhance remyelination, and significantly reduce disease severity in mouse models of MS.
Both drugs increased the number of new oligodendrocytes in brain slices from newborn mice. They also enhanced the generation of human oligodendrocytes from human OPCs in vitro. In a mouse model of MS, in which a toxin causes demyelination, administration of both miconazole and clobetasol promoted the repair of damaged myelin. Importantly, both drugs cross the blood-brain barrier. Administering each drug at the peak of disease resulted in a striking reversal of disease severity in the model animals. The researchers saw an increased number of newly generated oligodendrocytes, an increase in the extent of remyelination, and an improvement in function, with nearly all the mice regaining the use of one or both hind legs.
While both drugs promote remyelination, clobetasol also works to suppress the immune system. Miconazole appears to function directly as a remyelinating drug with no effects on the immune system.
Collectively, these results suggest miconazole and clobetasol should be tested as new therapeutic agents to enhance the repair of damaged myelin in MS patients. With more research and clinical trials in human patients, these drugs have the potential to treat the currently untreatable chronic progression of MS.